Scale tipping: Exploring obesity in modern rural Wisconsin
Hilary Gehin
Introduction
Clover pastures spread out like a carpet over rolling hills; outlining ghosts of once ubiquitous icebergs. The heavy smell of cow dung, drying corn, and fresh grass adds to the sense that time has turned back to an era of idyllic simplicity. Between stretches of cornfields, lush and ready for harvest, black and white spotted cows can be seen roaming back and forth, flicking their tails at flies. Behind them stands a proudly erected red barn kissing a tan silo. Nearby the barn rests a farmhouse; eggshell but with signs of achieving a ripe old age.
On the surface, Wisconsin farmland has the appearance of a landscape lush with fresh food and a healthy lifestyle. The truth however, is that citizens in rural areas are statistically older, have farther to driver to buy food, and live in food deserts that do not offer healthy options. Other factors, including education and poor infrastructure further contribute to the rise of obesity in Wisconsin.
The face of Wisconsin as you drive out of one of the major cities is idyllic in comparison to urban areas. Wisconsin boasts beautiful farmland that inspires nostalgia of the good ole’ days. This is in stark contrast to major cities, such as Madison or Milwaukee, that are as diverse as a Louisiana gumbo, and consequently face many issues common to other metropolises. In particular, large cities in Madison have food deserts, or areas where there is little to no access to farmers markets, grocery stores, or other venues that supply healthy food (American Nutrional Assoication, n.d.). Typically the only meal venues available in food deserts are fast food restaurants (American Nutrional Assoication, n.d.). Evidence has further shown that food deserts correspond to areas of lower socioeconomic statues. Lack of healthy food choices and an abundance of fast food restaurants in food deserts has led to health disparities, especially obesity, between the richer and poorer areas of cities (American Nutrional Assoication, n.d.). Obesity poses extreme health risks, including high blood pressure and cholesterol, diabetes, cardiovascular disease, stroke, osteoarthritis, and cancer (CDC, n.d.). In particular, cities such as Madison, Milwaukee, and Janesville have been mapped for the presence of food deserts within their cities. The maps clearly demonstrate that food deserts overlap with the known poorer areas of these municipalities (Madison.com, 2012).
Much research has focused on the impact of food deserts in poorer neighborhoods and cities, but little consideration has been given to food deserts in rural areas of Wisconsin. The food desert map in Madison for example shows a clear contrast between abundant food oases in down town Madison and food deserts beyond city limits. Considering that around 35% of Wisconsin residents live in rural areas, this issue is impacting Wisconsin citizens. Furthermore, with the rise in obesity rates in adults in Wisconsin it is imperative to determine what is causing this rise in obesity, and the role that food deserts in rural areas have in this health crises. Currently, Wisconsin ranks 14th out of all US states in obesity rate (Trust for America’s Health, n.d.).
Health experts agree that something needs to be done to address the obesity epidemic in America. Identifying the underlying causes of obesity prevalence in rural Wisconsin is the first step towards creating strategic communication to promote change within these communities.
Cultural Aspects of Rural Living
Rural areas are defined by the Census Bureau as “sparesley populated areas with fewer than 2,500 people” (USDA, n.d.). In Wisconsin, the state is mostly rural, with clusters of rural counties in the north and north-eastern areas.
While there are many differences between rural and urban living, both rural residents and those living in poorer city areas tend to have similar health challenges. In rural areas, there are aspects of the social environment that make efforts to improve public health particularly challenging. Rural residents “smoke more, exercise less, have less nutritional diets, and are more likely to be obese than suburban residents” (Unite for Sight). What hasn’t been studied in-depth is why these negative behaviors, particularly obesity, are being reinforced rather than discouraged with clear scientific data showing the risks of being obese. The underlying contributions to obesity in rural areas is the first step in creating strategic, culturally sensitive communication to promote healthy behavioral changes.
Findings*
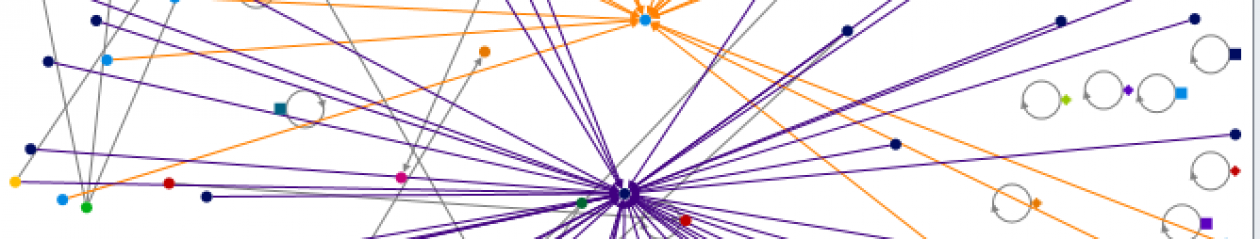
This map shows counties that were determined to be “rural” in Wisconsin according to the USDA Food Atlas. The US Census defines rural counties as being “non-urban areas,” which are densely populated and have a population of 50,000 or more. The obesity rate is depicted in red and the intensity of the color increases with obesity rate. Menominee stands out as the most obese county.
The average obesity rate in rural Wisconsin counties in 2010 was 30.0%, which was slightly lower than the national average (35.7%). The top ten most obese rural counties in Wisconsin are (from highest to lowest): Menominee, Dodge, Buffalo, Columbia, Trempealeau, Barron, Jefferson, Polk, Richland, and Kewaunee. All but Menominee has an obesity rate higher than Wisconsin’s average, but lower than the national average. Menominee’s obesity rate of 40.3% is over ten percent higher than the state’s average.
Of note are the four counties with a small population (2000-4000) that are also in the top ten most obese rural counties. These are: Richland, Trempealeau, Menominee, and Buffalo. Do these four counties represent key features of food deserts? Food deserts are defined by having fewer grocery stores, longer driving distance to grocery stores, and lower access to vehicles/transportation. How do the most obese counties in Wisconsin compare to the most healthy counties?
In Wisconsin, Walworth county has the lowest obesity rate, and the highest number of grocery stores. Though Pierce county has the highest population of all the counties, it has only 6 grocery stores. Menominee, with the highest obesity rate also has 6 grocery stores.
Looking at the percent of grocery stores per person, it is clear that the four rural counties with a small population and high obesity rate also have fewer grocery stores available. In addition, from 2007-2012, these four counties either had no change in grocery stores, or lost grocery stores (Menominee).
Exercise is just as important as diet in maintaining a healthy lifestyle and combating obesity. Noting patterns between recreational facilities and obesity rates in Wisconsin can determine if this factor plays a role in the obesity epidemic in this state.
The four counties with a small population and high obesity rate have four or less recreational facilities as of 2007. From 2007-2012, only Trempealeau saw an increase in recreational facilities, but they only gained one recreational facility. Menominee (originally with 0) and Buffalo (originally with 2) did not have any change in the number of recreational facilities and Richland, which was originally had four in 2007 had a 75% decrease.
Looking at all of the top ten most obese counties in Wisconsin, only two counties (Columbia and Trempealeau) saw an increase in recreational facilities from 2007-2012. All of the other eight most obese counties either saw no change or a decrease in recreational facilities.
Vehicle access and distance to grocery stores have been defined as key contributors to food deserts. Does Wisconsin see the same trends?
According to the USDA, “a tract is identified as having low vehicle availability if more than 100 households in the tract report having no vehicle available and are more than 0.5 miles from the nearest supermarket” (USDA, n.d.).
Focusing on smaller populated rural counties, it becomes clear that populations with higher obesity rates have more people living in households at least ten miles from the nearest supermarket/grocery store, more senior citizens living at least ten miles from the nearest supermarket/grocery store, and more people who earn lower incomes and are at least ten miles from the nearest supermarket/grocery store. In each of these cases, Oneida county is an outlier having a smaller population, but not one of the highest obesity rates.
Analysis
Taken together, this information points at the underlying causes of obesity in Wisconsin. Looking at the top ten most obese counties, they are similar in obesity rates but vary with the number of grocery stores, people per recreational facilities, vehicle access, and distance to the nearest supermarket. Two outliers, Menominee and Oneida, point to areas for further investigation and research.
Geographically, Menominee is a smaller count and is located within the heart of rural, north eastern Wisconsin. It has a low population (2,116 in 2010), very few grocery stores within the county limits (12), no recreational facilities, and the highest percentage of census tracts with low vehicle access and at least ten miles from any given household to the nearest supermarket. Menominee appears to represent the key issues of rural living on an exaggerated scale. While there is little variation between the other top ten counties in Wisconsin, Menominee has many factors putting its residents at risk for becoming obese. Coincidentally, Menominee’s population is composed of 87% Native Americans (Wikipedia, n.d.). This is consistent with previous studies that have found links between Native Americans and obesity risk.
On the other hand, Oneida county stood out as an outlier in that it has a small population, but its obesity rate is lower compared to other counties of similar size. Oneida has lower access to grocery stores for both the general population, seniors, and low-income residents, but it does have more grocery stores and recreational facilities than the top four smallest/most obese counties. Oneida county is extremely uniform racially, with a 97.7% white population.
Solutions
While the data appears to indicate a ominious future for rural communities, there is still hope. Cultural aspects of rural living can be used as an advantage in creating effective communication to promote behavioral changes. According to Philips and McLeroy: “Rural areas frequently have strengths including dense social networks, social ties of long duration, shared life experiences, high quality of life, and norms of self-help, and reciprocity” (2010). With this insight and theories of risk communication, doctors and other health officials could work towards informing rural communities the benefits of making healthier choices. Social norms have been found to greatly influence someone’s perceived risk (National Social Norms Center, n.d.). Creating campaigns that instill a sense that the norm is to exercise and eat healthy would be a challenge considering many rural residents are older and have long-established health habits. However, communicators could try to frame the message by showing the benefits of exercising/playing with your kids or grand children not only benefits your health, but helps keep a more concrete family bond. This would appeal to their cultural norm of having dense social networks and ties.
The concepts of self-help and reciprocity could also be utilized by health communicators. Because of driving distance and food deserts, rural residents might feel that they don’t have any means to help themselves eat healthier. In this case, establishing local farmers markets or community sponsored agriculture programs would be a way for people to feel that they have other food options besides gas station convenience stores and the sense of reciprocity, or supporting their neighbors who support them through providing fresh food would appeal to their cultural norms.
Conclusion
The data presented here points to key issues that are contributing to the rising obesity epidemic in Wisconsin. Focusing on the top ten most and least obese rural counties in Wisconsin, the correlations between obesity and grocery stores, recreational facilities, income, vehicle access, and distance to the nearest supermarket become clear.
In particular, rural areas are a major are of concern. With a higher population of elderly people who are less educated, more sedentary, and have restricted access to healthy food options, they represent a population that should be targeted for solutions to this health crises. Additionally, racial disparity appears to play a role in rural areas as well, with Menominee and Oneida as outliers with almost no racial diversity. In particular, Menominee stands apart as a county with the highest obesity rate with obvious causes. Located in the heart of rural Wisconsin with a majority population of Native Americans, Menominee has a small population, no recreational facilities, few grocery stores, low access to vehicles, and a majority of households at least ten miles from the nearest supermarket. Further studies looking at correlations between race and obesity rate would benefit from further investigating and comparing Menominee and Oneida.
There were several limitations to this study that are important to note. First, information for all counties in Wisconsin was not available. Furthermore, the latest set of complete data available was for 2010. Future studies should seek to find a more complete set of data for all rural counties in Wisconsin within recent years.
Behind the picturesque farms, the threat of obesity lingers within rural Wisconsin communities. As the younger generation leaves their family farms for the larger cities, they are taking with them the opportunity to promote change in their local community. Additionally, apparent racial disparities within rural counties points to deeper underlying aspects of rural food deserts.
These small counties are cautionary examples of what can happen to other counties if measures are not taken to combat the steady rise in obesity. By adopting the proposed solutions and conducting further research into other cultural aspects of obesity, Wisconsin can work towards becoming a state where cows, not scales, are being tipped.
*All data for this report was retrieved from: http://catalog.data.gov/dataset/food-environment-atlas
References
American Nutrition Association (n.d.). USDA Defines Food Deserts. Retrieved from: http://americannutritionassociation.org/newsletter/usda-defines-food-deserts
Center for Disease Control, (n.d.). Childhood Obesity Facts. Retrieved from: http://www.cdc.gov/healthyschools/obesity/facts.htm
Crowe, Kevin (2010). Many rural Wisconsin counties lost population since 2010. Retrieved from: http://www.jsonline.com/news/wisconsin/many-rural-wisconsin-counties-lost-population-since-2010-b99234138z1-252561011.html
Do Something (n.d.). 11 Facts About Food Deserts. Retrieved from: https://www.dosomething.org/facts/11-facts-about-food-deserts
Kaeding, Danielle (2015). For Rural Wisconsinites, Access To Food Can Be Difficult. Retrieved from: http://www.wpr.org/rural-wisconsinites-access-food-can-be-difficult
Madison.com (2012). Map: Madison’s Food Deserts. Retrieved from: http://host.madison.com/map-madison-s-food-deserts/pdf_fb7e1dec-cacd-11e1-ac43-001a4bcf887a.html
National Social Norms Center (n.d.). Social Norms Approach. Retrieved from: http://socialnorms.org/social-norms-approach/
Trust for America’s Health (n.d.). The State of Obesity in Wisconsin. Retrieved from: http://stateofobesity.org/states/wi/
Unite for Site (n.d.). Urban Versus Rural Health. Retrieved from: http://www.uniteforsight.org/global-health-university/urban-rural-health
USDA (n.d.). Retrieved from: http://www.ers.usda.gov/datafiles/Food_Access_Research_Atlas/Download_the_Data/Current_Version/documentation.pdf
Wikipedia (n.d.). Menominee, Wisconsin. Retrieved from: https://en.wikipedia.org/wiki/Menominee,_Wisconsin